Embargoed until 1 p.m. CT / 2 p.m. ET Tuesday, May 11, 2021
DALLAS and Washington, D.C., May 11, 2021 – Issued today, a new report from the American Heart Association (AHA) and the American College of Cardiology (ACC) on medical ethics and professionalism addresses important and timely topics in cardiovascular medicine including diversity, equity, inclusion and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems. The report is based on the proceedings of the joint 2020 Consensus Conference on Professionalism and Ethics and is published simultaneously in the AHA’s and ACC’s flagship journals Circulation and Journal of the American College of Cardiology, respectively.
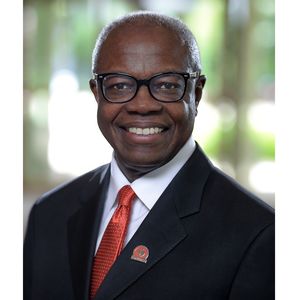
The AHA will present a live webinar and podcast series to amplify the report’s details, dialogue and actionable steps for cardiovascular and health care professionals, researchers and educators. The six-episode podcast series, “HEARTBEATS from Lifelong Learning: Professionalism & Ethics,” will be released weekly, starting on Tuesday, May 11, moderated by Co-chair of the Consensus Conference Report Ivor Benjamin, M.D., FACC, FAHA, a former AHA president, and featuring viewpoints from various cardiovascular thought leaders each week. On Thursday, May 13 at 11:00 am CT, Dr. Benjamin and former AHA President Robert A. Harrington, M.D., FAHA, will host a roundtable discussion webinar entitled, “Ethics and Professionalism: A Common Ground of Understanding.” The podcast series and roundtable discussion will explore perspectives that support robust ethical personal and professional behaviors and organizational actions and policies within the context of the current health care and scientific environment, as outlined in the Consensus Conference Report. The recorded webinar will be available On Demand.
The report’s details and recommendations will be presented and discussed this weekend in a session titled “Diversity and Equity: The Means to Expand Inclusion and Belonging,” on Saturday, May 15, at 8:00 am ET, during the American College of Cardiology’s 70th Annual Scientific Session.
The Consensus Conference Report presents a road map to achieving equity, inclusion and belonging among cardiovascular professionals that calls for continual assessment of the professional culture and climate, focused on improving diversity and achieving effective allyship. The report proposes continuous trainings to address individual, structural and systemic racism, sexism, homophobia, classism and ableism. The new report updates previous guidance the groups issued in 2004.
The report’s writing committee is a diverse group of cardiologists, internists and associated health care professionals and laypersons, organized into five Task Forces, each of which addressed a specific set of related topics. The five task forces addressed: conflicts of interest; diversity, equity, inclusion and belonging; clinician well-being; patient autonomy, privacy and social justice in health care; and modern health care delivery.
Recommendations for championing equity in patient care also include an annual review of practice records to assess for differences in patient treatment by race, ethnicity, zip code and primary language. The report suggests each health care setting conduct an annual review to ask, “How is racism operating here?” This review would examine structures, policies and norms and identify opportunities for intervention and improvement.
The AHA and the ACC reiterate their endorsement of the Principles of Professionalism published in 2002 in the Physician Charter on Medical Professionalism. Both organizations also reaffirm their commitment to social justice in the new recommendations.
“As much as 80% of a person’s health is determined by the social and economic conditions of their environment,” said Dr. Benjamin, who is also director of the cardiovascular center, co-director of the NIH T32 Postdoctoral Fellowship in Cardiovascular Sciences and professor of medicine at the Medical College of Wisconsin in Milwaukee. “To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of health equity lens for all.”
The report calls for a foundation of training in allyship and antiracism as part of medical school course requirements and experiences: a required course on social justice, race and racism as part of the first-year curriculum; school programs and professional organizations supporting students, trainees and members in allyship and antiracism action; and facilitating immersion and partnership with surrounding communities.
A section of the report is focused on the need for psychosocial support of the cardiovascular workforce, recommending that health care organizations prioritize regular assessment of clinicians’ well-being and engagement. Additional recommendations address the well-being of trainees and call for preventive and responsive mental health resources in post-graduate training programs. The resources should include an ombudsman program that allows for both confidential reporting of mistreatment and access to support. There is specific attention given to identifying “disruptive” or abusive behavior among medical teams and recommendations to ensure these behaviors are addressed regularly through professional training. Early career professionals and Fellows in Training were involved in this process.
The report details additional opportunities to:
- improve efficiency of health information technology, such as electronic health records, and reduce the administrative burden;
- identify and assist clinicians who experience mental health conditions, alcoholism or substance abuse, the prevalence of which is 2–14% among clinicians;
- emphasize patient autonomy using shared decision-making and patient-centered care that is supportive of the individual patient’s values;
- additional privacy protections for patient data used in research;
- guidance on maintaining integrity as new ways of delivering care emerge (e.g., telemedicine, team-based care approaches, physician-owned specialty centers);
- routine audits of electronic health records to promote optimal patient care as well as ethical medical practice; and
- expand and make mandatory the reporting of intellectual or associational interests in addition to relationships with industry.
“We have seen the COVID-19 pandemic challenge the physical and economic health of the entire country, coupled with a series of national tragedies that have awakened the call for social justice,” said Conference Co-chair C. Michael Valentine, M.D., MACC, FAHA, ACC past president and professor of medicine at the Heart and Vascular Center at the University of Virginia in Charlottesville. “There is no better time than now to review, evaluate and take a fresh perspective on medical ethics and professionalism. We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest, racial, ethnic and gender inequities and improve diversity, inclusion and wellness among our workforce. The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care.”
“The delivery of cardiovascular care is evolving rapidly. Through this evolution, our professional obligations to patient-centered care must remain steadfast,” said Dr. Benjamin. “How we engage and employ staff, receive payment, and provide and document patient care requires maintaining standards that are beyond reproach. We must maintain and promote integrity in all we do to protect public trust in science and medicine. Individuals and professional communities must take responsibility for evaluating and maintaining standards of care, while promoting an environment of diversity, equity, inclusion and excellence for all.”
Other organizations who had the opportunity to review and provide feedback on the report included representatives from the Heart Failure Society of America, the Preventive Cardiology Nurses Association, the American College of Preventive Medicine, the American Association for Thoracic Surgery, the American College of Physicians and industry.
The list of 40 volunteer committee members and co-authors, including their disclosures, are detailed in the report.
Additional Resources:
About the American Heart Association
The American Heart Association is a relentless force for a world of longer, healthier lives. We are dedicated to ensuring equitable health in all communities. Through collaboration with numerous organizations, and powered by millions of volunteers, we fund innovative research, advocate for the public’s health and share lifesaving resources. The Dallas-based organization has been a leading source of health information for nearly a century. Connect with us on heart.org, Facebook, Twitter or by calling 1-800-AHA-USA1.
About the American College of Cardiology
The American College of Cardiology envisions a world where innovation and knowledge optimize cardiovascular care and outcomes. As the professional home for the entire cardiovascular care team, the mission of the College and its 54,000 members is to transform cardiovascular care and to improve heart health. The ACC bestows credentials upon cardiovascular professionals who meet stringent qualifications and leads in the formation of health policy, standards and guidelines. The College also provides professional medical education, disseminates cardiovascular research through its world-renowned JACC Journals, operates national registries to measure and improve care, and offers cardiovascular accreditation to hospitals and institutions. For more, visit acc.org.
###
For media inquiries, please contact:
AHA: Michelle Kirkwood, michelle.kirkwood@heart.org, 703-457-7838
ACC: Dana Kauffman, dkauffman@acc.org, 202-375-6294






Leave a Reply